
Guide
Choosing a tool for automated triage and medical history
How can a healthcare organisation find the right tool in a jungle of different automated triage and medical history tools?
Introduction
Today, it is clearer than ever that healthcare workers must be able to use their time as efficiently as possible to help those who need it most. Therefore, it is no wonder that more and more healthcare organisations are realising the value of an automated tool for triage and medical history, which can compile patients’ symptoms and history and guide them to the right type of care.
Such a tool neither can nor should replace the important work of healthcare professionals. Nevertheless, it is important to ensure that it really adds the necessary value to support and streamline the work of healthcare professionals – both today and in the long term.
In a wilderness of different tools, how should a healthcare organisation navigate selecting the right one to work with?
We have listed a number of questions to consider when speaking to various suppliers (one of which will be getting some extra spotlight in this guide).
Start from scratch!
When the scope of what you want to achieve is that broad, it can be difficult to know where to start. The purchase or procurement of an automated triage and medical history tool is an investment that will affect the entire organisation – both the staff and the processes. It is critical to feel confident that you have made the right choice.
There is a number of questions that are important to answer:
- What do you want to achieve with the tool – today and in the future?
- How does the tool work?
- Can the tool be integrated with existing tools? If so, how?
- How many symptoms and diagnoses can the tool handle?
- How much ongoing work will the tool demand from your healthcare organisation?
- Can the tool handle several different areas of care or only primary care?
- Is it possible to connect the tool to other systems and data sources?
- Is the tool flexible, i.e. can you customise functionalities based on your needs?
- How does the tool ensure the quality and validation of the results?
The very first question one should ask is:
What do you want to achieve with the tool – today and in the future?
It is important to clearly formulate which issues you expect the tool to address. Do you need aid on a general level within primary care? Or do you prefer a tool that can eventually be used in more areas, handle more complex cases, and could eventually be used more autonomously to guide the patient in the right direction?
The potential of such a tool is closely linked with the technological architecture it is developed on. This automatically leads us to the next question, which will be a large area of focus in this guide:
What model is the tool based on?
This question should be asked early on in the selection process, as it is immensely revealing for the possibilities and limitations of the tool. But first, here is some information on a few popular models:
Rule-based expert systems
Most automated triage and medical history tools are currently based on a so-called rule-based expert system (sometimes also called decision trees or structured questionnaires). Several Computer Decision Support Systems (CDSS) are widely used across the NHS either for risk assessment, ambulance services, or prescription support for GPs. In an automated tool based on this model, patients answer questions according to a yes/no, over/under etc principle. Depending on the response, they proceed to various predetermined branches in the tree, based on different scenarios and connections entered into the system.
A rule-based expert system has its advantages. It is clear, transparent and can be optimal in situations involving relatively simple problems and tools.
However, keep the following points in mind:
- Every conceivable scenario must be pre-entered into the system
The need to manually enter and maintain thousands of possible scenarios into the system not only places high demands on the people tasked with describing all these scenarios – it also entails a massive amount of work that costs time and money.
- It is only possible to deal with only one symptom at a time
Patients rarely have only one symptom. There are often many parallel symptoms, all of which must be taken into consideration. In addition, if it is possible to select only one symptom, it can be difficult for patients to decide which one to choose, which often means that they will enter ‘Other’ just in case – a path that few tools can handle.ool will overgeneralise instead of operating in a custom and patient-centric way.
- It is not possible to change course
The structure of the model limits the ability of users to change course once they have selected a certain path.
Things don’t always follow a straight line: what initially seemed to be gastritis might instead be a problem linked to mental illness. Unlike a rule-based expert system, a nurse who provides advice over the phone can easily change paths once she/he realises this. Predetermined scenarios entail the risk that the tool will overgeneralise instead of operating in a custom and patient-centric way.
- The model demands a great deal of human involvement
Once again, it is important to emphasise that an automated tool neither can nor should completely replace healthcare professionals. But a tool based on a rule-based expert system will require a relatively large amount of human involvement – people who can think past certain bends in a path or find the right way forward when they encounter a dead-end. In the long term, this limits the possibility of automating parts of processes and/or decisions.
So, what are the alternatives?
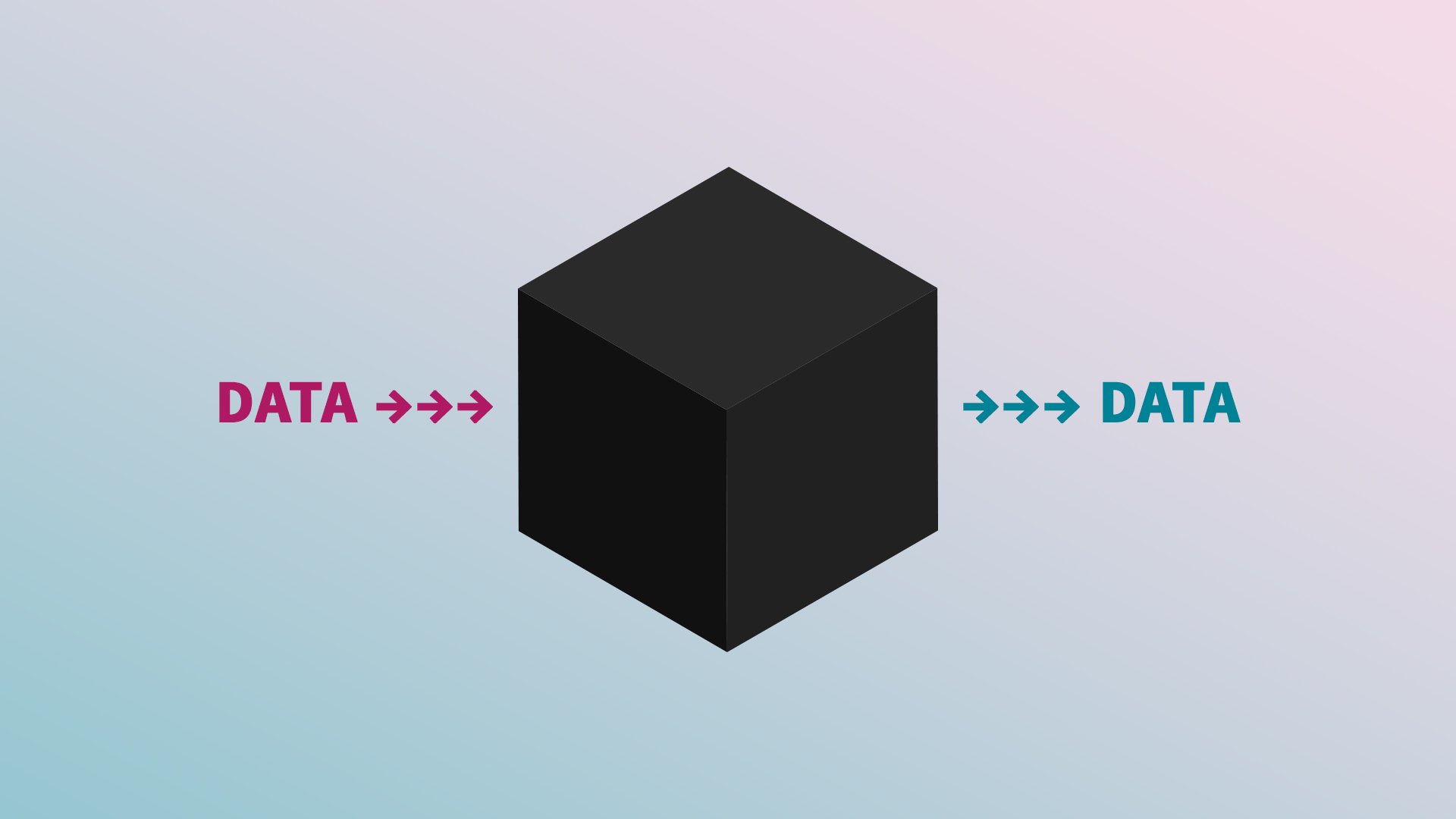
Black box
One alternative model is Black box – an AI or Machine Learning model, that has been used in healthcare for many years. A Black Box tool can identify patterns within vast amounts of data and is used, among other things, to identify images in radiology. In this model, you submit data and receive data – however, you do not know how and why specific data is generated. This lack of transparency makes the application of this model to triage and medical history problematic. As security is crucial in these tasks, it is important to have the ability to retrace how a conclusion has been drawn.
Probability-based network
A third model in automated triage and anamnesis is a so-called probability-based network, also known as a Bayesian or probabilistic network.
A probability-based network does not need a great deal of data from the start — the important thing is that the right type of data is added, i.e. validated data based on expertise. The network also has rules about how diagnoses and symptoms relate to each other. The likelihood of various conditions can be dynamically evaluated following each response provided by the patient. Humans can enter data and rules, but, after that, it is up to the algorithms to work out answers and probabilities. The conclusions of the algorithms are then validated and entered as new data.
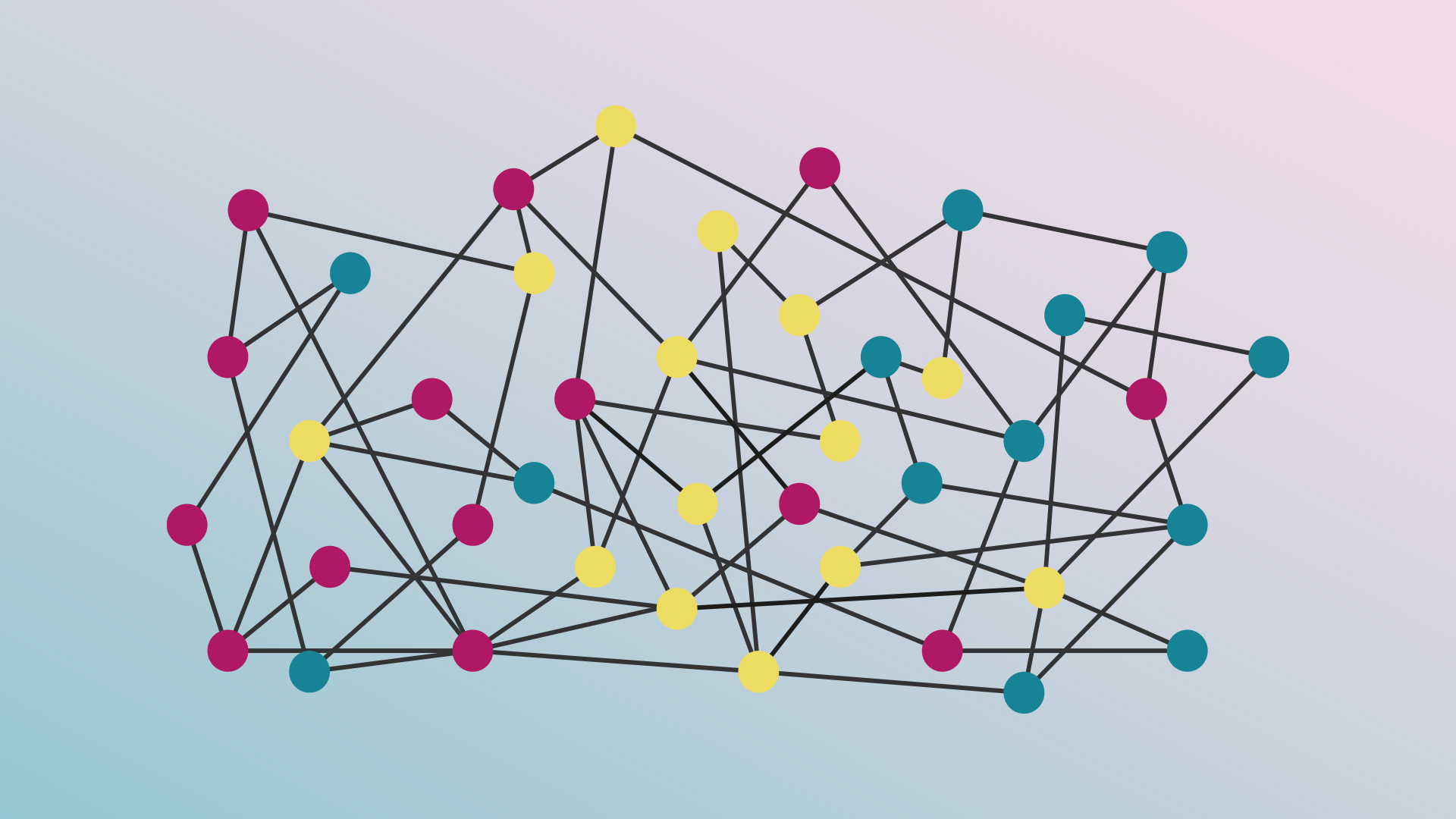
In a tool built on a probability-based network, patients can still answer questions about their condition and medical history. However, unlike a rule-based expert system, which is limited to a specific tree and its various branches, such a tool can retrieve information from the multitudes of different nodes and rules that exist within the network. Depending on the responses provided by the patient, new relevant follow-up questions can be identified and displayed for the patient, while the likelihood of various conditions can be dynamically evaluated following each patient response. A patient can come in with several symptoms, and the more information the patient adds with every response, the more nodes are connected. This affects both follow-up questions and possible diagnoses. This way, the model has a completely different basis for handling more complex cases, compared to rule-based expert systems.
The advantages of choosing an automated tool based on a probability-based network include:
- Processing millions of different scenarios
There are virtually no limits to how many symptoms and diagnoses can be included in a probability-based network — it can handle millions of different scenarios. In addition, the network can take into account a patient’s addition of one or more parallel symptoms from the outset, but it can also change course when information is added or altered. All specified information is taken into account, as well as relationships between symptoms and different conditions.
The model also affords full transparency and can explain why different conclusions have been drawn – a key point in patient-centric care and safety.
- It gets smarter over time
By continuously adding more information and test-driving various parts of the network, users can help the network get smarter over time. Since it is possible to both suggest suspected diagnoses and provide advice, decisions become more reliable over time. This means that an automated tool based on this model has the potential to act autonomously in certain cases (for example by recommending self-care to patients), provided that sufficient amounts of data are collected and decisions are sufficiently validated.
- It can be connected to other relevant data sources and networks
In a probability-based network, the system can include other relevant data sources. This may include data from, e.g. a smartwatch and other monitoring tools which can provide information about heart rate, movement, sleep patterns, and more. However, such a system can also collaborate with other major types of networks, such as networks that specialise in skin conditions or can track the spread of infection with the help of a user’s GPS location. The possibility of collaboration with other networks does not just mean that the areas to include can be potentially limitless – it also makes the tool future-proof. After all, it is impossible to know what the demands of the market will be in ten years’ time, and no single organisation or supplier can solve everything. With an open system, you can incorporate whichever parts are in demand.

- It requires minimal maintenance by your organisation
A probability-based network is continuously improved, as users ‘feed’ it with new validated data. But unlike a rule-based expert system, it does not require a human to describe every possible process in detail, or rewrite the content, when the information is changed or needs to be supplemented. The connection itself handles the algorithms. This eliminates the need for organisations to invest large amounts of time (and money) building up content until it is ready for use.
A relevant example: In the event of a sudden pandemic, the tool needs to ask new questions and make new connections in order to produce relevant diagnoses. In a rule-based expert system, these trees and branches would need to be added from scratch, while all existing trees would need to be updated to account for the new information. In a probability-based network, one merely needs to add a number of new risk factors, symptoms and diagnoses. This means that there is no need to build – or, if necessary, change – the content. Instead, one can simply reinforce the existing system by adding new relevant data.
In the above question and description, we have conveniently touched upon a number of the questions in our list:
- How many symptoms and diagnoses can the tool handle?
- How much work will the tool demand from your healthcare organisation?
- Can the tool handle several different areas of care, or only primary care?
- Is it possible to connect the tool to other networks and data sources?
However, there are a few remaining questions:
How does the tool work?
The underlying structure can provide information about how the tool works on the back-end, but it is also important that the tool works well for end-users. Healthcare professionals need a flexible and intuitive system, apt to provide the information and structure necessary to save time and work more efficiently while ensuring patient safety. But patients’ needs must also be met – if they are not satisfied with the tool, or if they do not trust it, they will most likely find other ways to contact their healthcare providers. Therefore, ask the supplier to review the functionality of the tool in detail, so that you can see flows from different perspectives. It is a good idea to ask whether user tests involving both healthcare professionals and patients have been conducted, and what processes have been set up to ensure user-friendliness.
Can the tool be integrated with existing systems?
Working in parallel systems is hardly sustainable in the long run. Make sure that the tool is open for integrations with your existing systems.
Is the tool flexible?
Not all healthcare organisations work in the same way, and there is great value in the ability to choose or customise functions based on your own needs. It is then valuable to find out the configuration capabilities of the tool.
How does the tool ensure the quality and validation of the results?
Find out which processes and guidelines the tool uses to ensure quality and validation. What does the process look like? How is the content validated? It is important that you find the tool to be safe and secure.
In this guide, we have compiled various points to keep in mind as you begin to search for possible tools for automated triage and medical history.
Don’t hesitate to contact us to exchange ideas or discuss how various tools work.